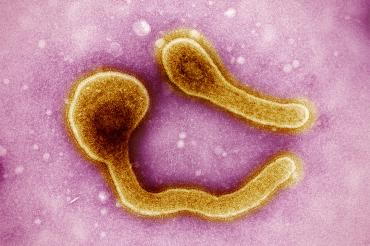
Lessons learned during Ebola crisis can help manage Marburg outbreak: U of T expert
Published: March 23, 2023
Earlier this year, Equatorial Guinea declared its first outbreak of Marburg virus disease, with 11 confirmed deaths so far.
The Marburg virus – a rare but severe hemorrhagic fever which affects both people and non-human primates – belongs to the same family of viruses as Ebola. The disease presents with similar symptoms, including high fever, diarrhea, abdominal pain and cramping, and occasionally severe bleeding.
Rob Fowler, a critical care physician at Sunnybrook Health Sciences Centre and a professor in the department of medicine at the Temerty Faculty of Medicine at the University of Toronto, volunteered with the World Health Organization (WHO) on the frontlines of the Ebola outbreak in West Africa in 2014 and in Congo in 2018. In 2021, he co-chaired the WHO guideline development group that published the first guidelines for Ebola virus disease therapeutics.
He recently spoke with writer Betty Zou at the U of T-based Emerging and Pandemic Infections Consortium (EPIC) about the recent Marburg outbreak and what lessons health professionals can learn from the prior Ebola crisis to help manage this infectious disease.
What do we know about Marburg virus and how it’s transmitted?
Marburg is typically spread from an animal reservoir to other animals or to humans. When it gets into humans, there can be human-to-human spread through direct contact. The direct contact is often through bodily secretions, such as someone vomiting, having diarrhea or bleeding.
Once the virus gets onto a person’s hands, it can enter the body through mucus membranes like your eyes or the inside of your nose and mouth. In rare instances, we’ve seen health-care workers get infected through a needle-stick or sharps injury in the skin that allows the virus to directly enter the blood. And very, very rarely, people have found residual virus in certain bodily fluids that evade the immune response after the acute infectious phase has passed.
How did you react when you first found out that the cluster of people who died of suspected hemorrhagic fever had tested positive for Marburg virus?
Any time there’s a Marburg outbreak, it’s worrisome. Historically, it’s a virus that spreads efficiently from person to person and the mortality has typically been very high.
Like Ebola, this virus often shows up in areas that have underdeveloped health-care systems and a lot of characteristics within society at large that enable person-to-person spread. Tight living quarters is one example. These areas oftentimes don’t have the ability to limit virus spread because of a lack of access to consistent running water. So Marburg or Ebola outbreaks are, of course, very tough for patients and health-care teams, but also very difficult for the health-care system and the population at large to manage.
I feel for the folks that are in the thick of it right now because it’s very, very hard.
What lessons can we take away from the Ebola outbreaks over the past decade to respond to the Marburg virus disease outbreak?
When you have a disease that has a high mortality rate – mortality for Marburg virus disease can range from 25 per cent to 90 per cent – and is very transmissible, we really need to focus on prevention and trying to stop the outbreak from getting larger.
If you’re not living in an area where clinicians are able to send samples for rapid testing, then you can get behind very quickly in an outbreak. Having reference testing laboratories that are geographically nearby is critical. It’s also really important to have a culture of infection prevention and control embedded in health-care settings. The same precautions we use to prevent norovirus transmission in Canada would work well to protect people from more serious viruses like Marburg and Ebola.
If we can provide health-care teams with basic precautionary tools – gloves, gowns, eye protection, medical masks, access to running water and soap – combined with well-practiced infection prevention and control hospital processes, then that will help to prevent spread within health-care facilities.
Another key element is clear and effective messaging to the public about how we can prevent spread in the community. In addition to excellent infection prevention and control practices in hospital, you also need equal engagement in the community where the virus can otherwise spread.

Rob Fowler, second from right, with WHO colleagues, clockwise from bottom left: Sharmistha Mishra, Benon Tumwebaze, Senyonga Muzafalu, Adrienne Chan, Peter Kiiza and Mekonnen Tadesse at the Ebola Clinical Training Centre in Freetown, Sierra Leone (photo courtesy of Rob Fowler)
Where are we with vaccines and treatments for Marburg virus disease?
There currently isn’t an approved vaccine for Marburg virus. However, there are a number of promising early-phase evaluations underway. Having an effective and accessible vaccine is key in terms of prevention of infection.
For treatments, there are nonspecific antiviral medications that may be effective – including repurposed medications such as remdesivir, which has been used to treat people with COVID-19 and tested previously in Ebola virus outbreaks.
Important products in development include monoclonal and polyclonal antibodies that are specific to the Marburg virus. In our experience with Ebola, those antibody treatments were incredibly effective in reducing mortality. For Marburg, that probably represents one of the brightest hopes. To develop these antibodies, there has to be a will – not just medical or societal will, but an economic will – to do it. For Ebola, that economic will existed during and after the 2014 outbreak in West Africa. For Marburg, there has been less of an economic imperative for companies to dive into this, but hopefully that changes.
One of the things that the WHO can do is bring people together from academia, industry and other sectors and set priorities that help to send a signal and direct funds. That has happened recently for Marburg and now there are more candidate drugs being tested. I think there’s lots of hope that, as with Ebola, Marburg will have effective therapies.
What’s your outlook on this current outbreak?
It’s hard to share predictions being so far away from what’s happening on the ground, but I think it’s fair to say that we’re never out of a danger zone when an outbreak is ongoing. Sometimes you have an initial surge of cases being diagnosed, followed by concern among the public and people not seeking care or not getting tested out of fear. That can create a lull between the first set cases and the next bump in cases. The incubation period is usually about a week, but can be up to about three weeks.
Theoretically, if you go three weeks without a new case, you might think that the outbreak is clearing. However, that assumes you know about all the new cases – which is almost never true. There’s a relatively large risk that there will be unknown cases. That’s why we generally go through at least two 21-day periods without a new case before we think an outbreak is over.
How can the EPIC community help respond to outbreaks like this one – now and in the future?
There’s so much expertise in the EPIC community – and in the Toronto and Canadian communities more broadly. I think we really have had an outsized influence on vaccine and therapeutic development, diagnostic testing and clinical care.
Canada has been a leader in developing vaccines and monoclonal antibody treatments that were very helpful during the 2014 Ebola outbreak in West Africa. Supporting lab-based diagnostic capacity in Africa was also incredibly helpful. The National Microbiology Lab in Winnipeg has been very good at supporting other countries and helping them build up their diagnostic capacity.
Canadians have helped to build the foundations of excellent acute and critical care for patients with Ebola – this goes such a long way to reduce mortality even when there isn’t a specific therapy available. Yet, all of this requires people to say that it’s not just someone else’s issue – it’s our collective issue that we can bring our expertise and resources to help with. It’s about individual people asking themselves the question, “Do I have something to offer?” The answer is almost always, “Yes.”



