Microfluidic device reveals how tumour shapes can predict cancer aggressiveness

Associate Professor Edmond Young of U of T's Faculty of Applied Science & Engineering (left) and PhD alum Sina Kheiri co-developed the Recoverable-Spheroid-on-a-Chip with Unrestricted External Shape – or "ReSCUE" – platform (photos courtesy of Edmond Young and Sina Kheiri)
Published: December 18, 2024
Researchers in the University of Toronto’s Faculty of Applied Science & Engineering have designed a microfluidic platform that can be used to predict cancer cell behaviour and aggressiveness, opening up new avenues for personalized and targeted cancer treatment.
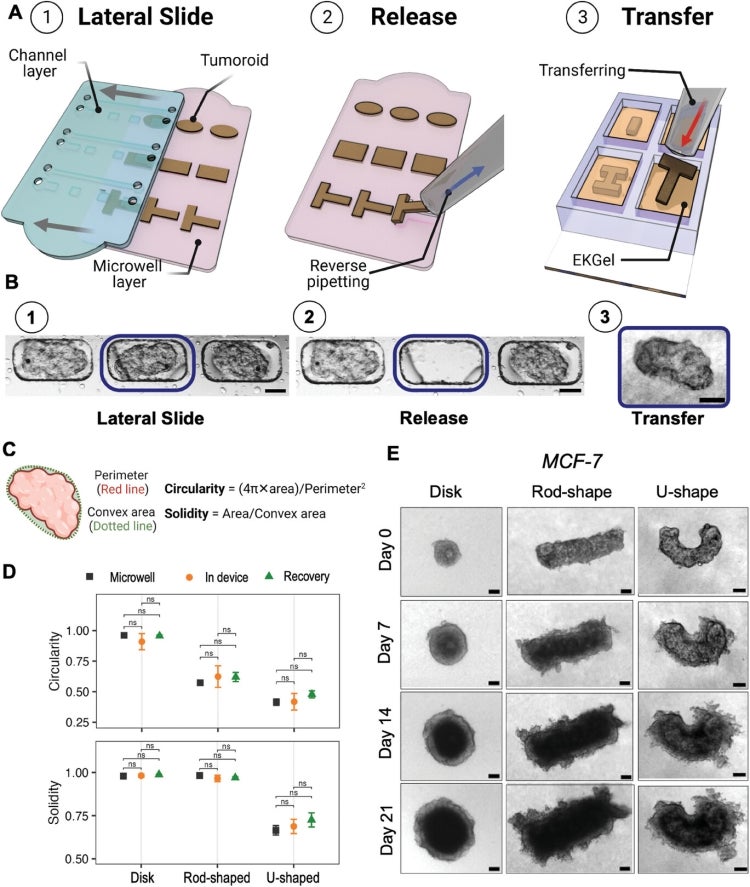
The Recoverable-Spheroid-on-a-Chip with Unrestricted External Shape (ReSCUE) platform, developed by a team led by Edmond Young, an associate professor in the department of mechanical and industrial engineering, gives researchers the ability to recover and release tumoroids – tumour cells derived from patients – to perform downstream analysis and characterization.
This allows for unprecedented control and manipulation of tumour shapes, a largely unexplored area in cancer research.
“While there are several platforms for in vitro modelling of spheroids – three-dimensional aggregates of cells that can mimic tissues and mini tumours – a challenge in the cancer research field has been the inability to control the shape, recovery and location of these cancer organoids,” says Sina Kheiri, a PhD alum and co-lead author of the study, which was published in Advanced Materials.
“So, researchers end up with these tumours-on-a-chip that can’t be easily characterized because they are stuck on the device and can only be observed through optical microscopy.”
The platform also enables researchers to grow cancer organoids in different shapes. This is important, Kheiri says, because much of the current research on cancer cell in vitro modelling is focused on spherical tumours, but tumours in a body can take many different shapes.
“In many invasive cancers, the tumour shape is not spherical. For example, in a recent study of 85 patients with breast cancer, only 20 per cent of tumours were spherical,” he says. “If modelling studies are limited to spherical tumour shapes, then we are not looking at the full parametric space and scale of tumours that are seen in real life. We are only looking at a small portion of the whole answer to understand cancer cell behaviour.”
Kheiri’s PhD research was co-supervised by Young and Eugenia Kumacheva, a professor in the Faculty of Arts & Science’s department of chemistry who is cross-appointed to the Institute of Biomedical Engineering. Kumacheva’s lab developed a biomimetic hydrogel that is used as a scaffold in the multi-layer ReSCUE platform, allowing the patient-derived cancer cells to grow and organize the way they would inside human tissue.
The platform was developed in collaboration with David Cescon, a clinician scientist and breast medical oncologist at Princess Margaret Cancer Centre and associate professor in the Institute of Medical Science at the Temerty Faculty of Medicine. Cescon’s team provided access to the cancer cells that were used to form breast cancer organoids.
The idea that tumour shapes determine cancer cell behaviour was a serendipitous discovery for Kheiri: while optimizing and developing the microfluidic platform, he discovered that some of the patient-derived tumoroids were forming positive curvatures because of the shape of the microwell.
“I was playing with the aspect ratio of the microwells and observed that when the wells had a more rod-like or elongated shape, rather than a circular or disc shape, the tissues formed cellular strands at the regions with positive curvature,” he says. “I didn’t see that in tumoroids from the same cancer-cell sample that formed a spherical shape.
"So, we started to make different shapes and analyze the effects of shape or curvature on cancer behaviour."
The team looked at disk-, rod- and U-shaped tumoroids; they found higher cell activity and higher proliferation at the positive curvatures – where the tumour shape is convex and outward curving.
This could mean that the growth of cells in these areas is more invasive compared to areas of the tumour that have a flat curvature.
“Understanding the relationship between tumour shape and cell behaviour is important for predicting tumour aggressiveness and planning appropriate treatment strategies, such as targeted radiation therapy or drug delivery,” says Kheiri. “We want to open this door and give researchers a platform that they can use to study how different tumour shapes respond in anti-cancer drug treatment, in radiotherapy and chemotherapy.”
Now a postdoctoral researcher at the Massachusetts Institute of Technology (MIT), Kheiri continues to provide support to the Young lab on development of the ReSCUE platform. The researchers recently submitted a U.S. patent and are looking to build on their results.
“We hope that these uniquely shaped mini tumours can help biologists and cancer researchers better understand the biology of cancer cells and how they respond to drugs,” says Young.
“We’re going to add even more complex features, such as surrounding vasculature. The more control we have over the features we can include in our models, the more realistic they become, and the more accurate our drug testing will be.”



